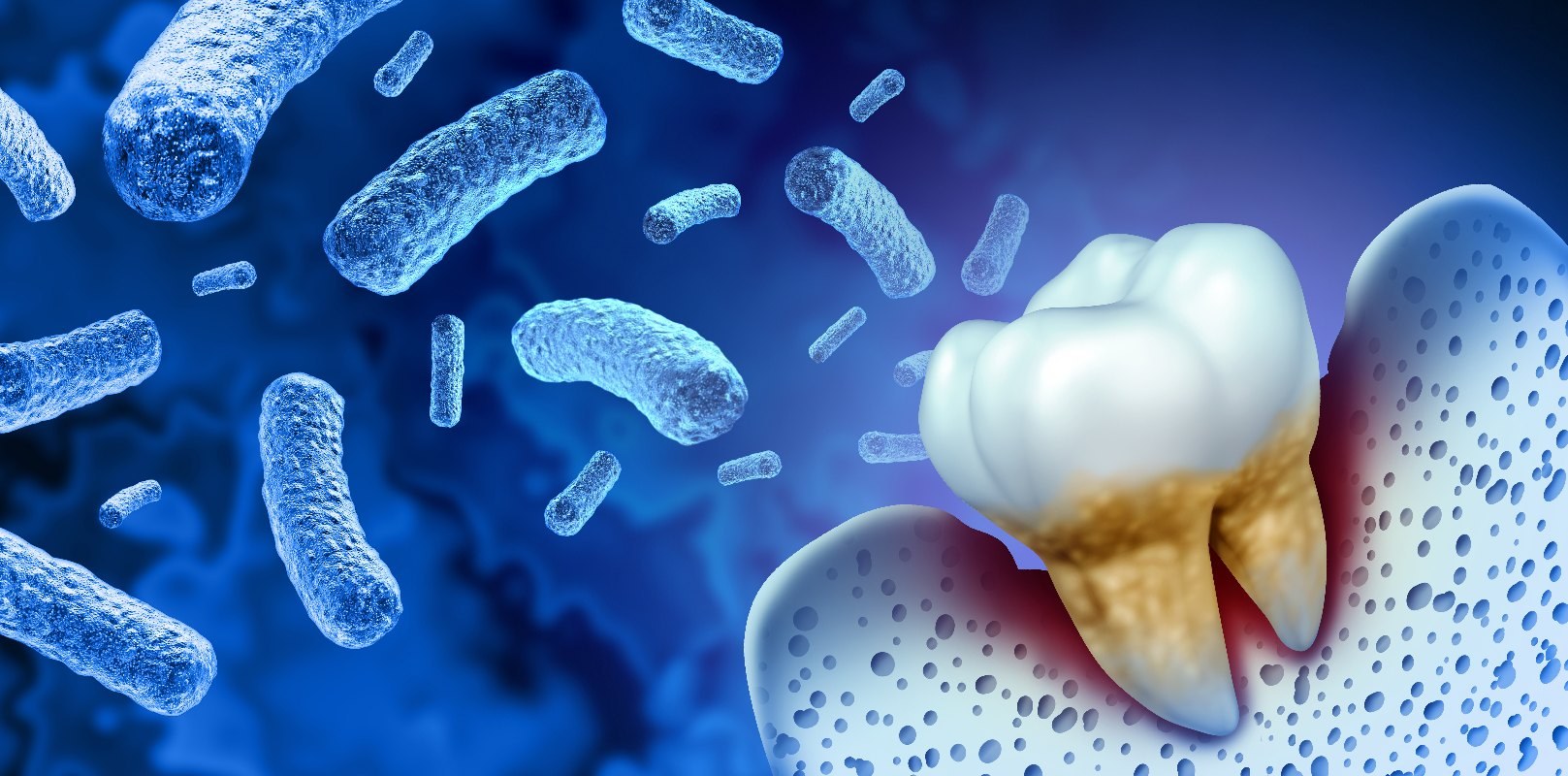
Periodontitis is a bacteria-induced tooth-bed inflammation. Older dental patients may know this as periodontal disease. The socket of the tooth, i.e. the layer of bone, connective tissue and gums, which is located under the tooth, is called periodontium.
What is periodontitis?
The periodontitis-causing bacteria come from the normal oral flora. They colonize the food debris and saliva plaque and excrete toxins and acids that are so aggressive that they even attack the gums. It then becomes gingivitis. If they penetrate to the jawbone, it is called periodontitis.
Dentists assume that the bacteria originating from the infected gums even reach other parts of the body: it was already possible to detect various types of periodontitis bacteria in the human coronary arteries.
A periodontal disease always runs painless in the initial stage disease, so that the affected do not even know that they are sick.
What forms of periodontitis are there?
Peridontology (the medical specialty that is dedicated to the periodontal ligaments) distinguishes the following forms:
- Chronic periodontitis. It usually occurs in adults and progresses only slowly.
- the aggressive periodontitis. In this the inflammation in the jaw spreads faster. It also occurs in adolescents.
- the apical periodontitis. With this, the inflammation is near the tips of the tooth roots (apex). It leads to the dissolution of the jawbone and the formation of cysts (fluid-filled tissue capsules).
For each of the forms of periodontitis other bacterial strains are responsible.
What are the causes of periodontitis?
The main cause of inflammation of the periodontium is inadequate oral hygiene: the sufferer does not brush his teeth frequently and / or thoroughly enough. In addition, many of those with periodontitis sufferers are among those who receive dental examinations only sporadically. Thus, the pathogens in the oral cavity have ample opportunity to multiply rapidly and to settle on biofilm (dental plaque) and tartar.
Other causes of periodontitis include:
- Malnutrition (too many sugary foods)
- obesity (obesity)
- Diabetes, rheumatoid arthritis (joint inflammation)
- osteoporosis
- untreated gingivitis
- a weakened immune system(especially in patients with HIV /
- an inherited predisposition AIDS):A certain genetic Defects disturb the immune system, so that the body produces an excess of messenger substances (cytokines) such as interleukin-1-alpha and interleukin-1-beta. They additionally increase the inflammation in the body and accelerate the degradation of the tissue.
- other genetic diseases such as Down syndrome and hypophosphatasia (phosphate deficiency)
- heavy smoking: The nicotine reduces the gum circulation, so that it is no longer adequately protected by the immune system.
If you suffer from any of the listed underlying conditions or are a heavy smoker, it is important to take regular dental check-ups with a specialist in dentistry. This way, any existing inflammation can be treated in good time.
Symptoms and course of tooth-bed inflammation
The inflamed and reddened gums swell and form gum pockets: The usually very narrow gaps between the gums and the tooth become larger and fill up with bacteria and pus. This makes it increasingly difficult to clean your teeth. It comes after daily oral hygiene more often to bleeding gums and secretion of pus in the mouth.
As the aggressive pathogens also attack the jawbone, the gums will recede. The necks are free and sensitive to pain. In addition, they react intensively to cold and warmth. Due to the damaging influence of the bacteria, the jawbone retracts as well. Since the pathogen excretes unpleasant-smelling metabolism products, the periodontitis patient stands out due to strong bad breath. Stronger bone loss causes additional tooth loss: The retracting jaw bone ensures loose teeth.
Diagnosis of periodontitis
If the dentist suspects that his patient is suffering from inflammation of the periodontium apparatus, he then examines the gums and teeth more precisely. He inserts the periodontal probe into the gum pockets and measures how deep they are already. Using an x-ray, he recognizes how the teeth sit in the jaw. In addition, he can use the X-ray image to better assess bone degradation processes. This is especially true for the otherwise not easily diagnosed apical periodontitis. He sees if 1, 2 or 3-walled or bowl-shaped bone pockets have formed.
The specialist in periodontology then uses special dental instruments to take samples of bacteria from the gum pockets and analyze them in the laboratory for their composition. The test result then provides him with the information he needs for efficient treatment of the patient: which bacterial species have triggered the present dental calcareous inflammation.
How to treat periodontitis
Often it is enough to thoroughly cleanse the patient's teeth with a professional tooth cleaning (PZR) and to encourage him to take care of his teeth more thoroughly in the future. He finds out in a special consultation with the dental specialist which dentistry techniques are most suitable for this. In general, the appropriate toothbrush, interdental brush (for interdental spaces) and dental floss are already sufficient for this. In addition, the patient can stem the multiplication of the pathogens with the regular use of a disinfecting mouthwash and a tongue scraper.
If the periodontal disease is already well advanced, the dentist performs a curettage: Using certain surgical tools such as scalers and curettes or the ultrasound device, he scrapes off all the bacterial deposits in the periodontal pockets. Because the treatment is quite painful, the patient is previously given a local anesthetic. If the inflammation persists, an open curettage is required: the periodontist will surgically separate the gingival margin from the teeth and jawbone to better process the tissue pockets and remove infected gums.
Particularly aggressive bacteria can only be eliminated with antibiotics. However, there are only a few drugs in question, as the pathogens are within the biofilm and therefore less responsive to the drug.
Patients with periodontitis who are willing to pay for their own therapies that are not covered by statutory health insurance have the option to undergo laser treatment. The special devices work with specific wavelengths or chemical substances that react to light, effectively killing all pathogens. The innovative treatment methods save the patient the painful open curettage despite the anesthetic. In addition, they have the advantage that the wounds heal faster and rebleeding occurs less frequently. After therapy, the patient is then given anti-inflammatory and bacterial growth-limiting drugs.
Weitere Beiträge

Toothless jaw
Carefree smile and laughter without teeth - unthinkable. Even speaking without teeth is a real challenge for both the speaker and the listener. Last but not least, the food is no longer enjoyable, because a toothless jaw fulfills the chewing function only inadequately.